
Mental health billing is rarely straightforward. Services overlap. Providers work as teams. Sessions happen in offices, hospitals, schools, and homes. Add telehealth into the mix, and billing can feel like juggling glass plates. This is exactly where modifiers step in.
Modifiers do not change what service you provided. They explain how, by whom, where, and under what conditions the service took place. In behavioral health, that context is everything. When modifiers are proper, claims glide through. When they are wrong or missing, denials follow like clockwork.
This guide pulls together the most important behavioral health modifiers and explains them in a way that actually makes sense. No coding dictionary language. Just real-world clarity for providers, billers, and practice owners.
What Are Behavioral Health Modifiers?
Modifiers are two-character codes added to CPT or HCPCS codes on insurance claims. They give payers extra details that the base code alone cannot provide.
In behavioral health, modifiers often clarify:
- The provider’s license or credential level
- Whether care was delivered via telehealth
- If services were separate or distinct on the same day
- Whether care was part of a specific mental health or substance use program
Think of modifiers as footnotes to your CPT code. Without them, payers may misread the story behind the service.
Why Modifiers Matter More in Behavioral Health
Behavioral health services are layered by nature. A single patient might receive therapy, medication management, and crisis support from different clinicians in one day. Modifiers help insurers understand that complexity.
Correct modifier use:
- Prevents automatic denials from bundling edits
- Ensures payment at the correct rate based on provider credentials
- Supports medical necessity when services exceed limits
- Reduces audit risk, especially for high-frequency therapy
In short, modifiers protect both reimbursement and compliance.
Behavioral Health Modifiers You Must Know
Modifier 25 – Separate and Significant E/M Service
Modifier 25 is used when an Evaluation and Management service is provided on the same day as psychotherapy, and the E/M work exceeds routine assessment.
Common example:
A psychiatrist adjusts medications and also delivers psychotherapy during the same visit.
What trips practices up is overuse. A quick medication check baked into therapy does not qualify.
Strong documentation is key. The E/M portion must stand on its own.
Modifier 59 – Distinct Procedural Service
Modifier 59 informs the payer that two services that are usually bundled together were actually separate.
In behavioral health, this often applies when:
- Individual and group therapy occur on the same day
- Services happen at different times or in different settings
This modifier should never be your first instinct. If a more specific modifier applies, use that instead.
X Modifiers (XE, XP, XS, XU)
These are refined alternatives to modifier 59 and are preferred by many payers.
- XE – Separate encounter
- XP – Separate practitioner
- XS – Separate structure
- XU – Unusual, non-overlapping service
For behavioral health, XE is the most common. It shows services occurred in distinct sessions, not just back-to-back.
Telehealth Modifiers in Mental Health
Telehealth is no longer a temporary solution. It is a core delivery method in behavioral health.
Modifier 95 – Live Video Telehealth
This modifier signals synchronous audio and video services.
It applies to psychotherapy, diagnostic evaluations, and medication management when delivered via real-time video.
Most payers still require the correct Place of Service code along with modifier 95.
Modifier GT – Telehealth (Legacy Use)
Some commercial payers and older Medicare policies still accept GT.
Always follow payer-specific rules. Using the wrong telehealth modifier is a common denial trigger.
Modifier 93 – Audio-Only Services
Modifier 93 applies when services are delivered by telephone without video.
This is especially common in behavioral health, but coverage is limited. Many payers allow it only under specific conditions.
Your documentation must explain why the video was not used.
License and Credential Level Modifiers
In behavioral health billing, who delivers the service matters just as much as the service itself. Many claims are approved or denied purely based on the provider’s license level. This is especially true for Medicaid and managed Medicaid plans, where reimbursement rules are tightly tied to credentials.
License-level modifiers clearly convey the clinician’s qualifications to the payer. Without them, payers may assume the wrong provider type, apply the wrong fee schedule, or deny the claim outright.
Modifier AF – Psychiatrist (MD or DO)
This modifier is used when a psychiatrist performs a service. It signals that the provider is a medical doctor with prescribing authority. Many payers reimburse higher rates for AF because psychiatrists can deliver both medication management and psychotherapy. If this modifier is missing, payers may downcode or deny services tied to medical decision-making.
Modifier AH – Clinical Psychologist
AH identifies services provided by a licensed psychologist. Psychologists often bill diagnostic evaluations and psychotherapy, but do not prescribe medications. This modifier helps payers apply the correct coverage rules and reimbursement rates specific to psychology services.
Modifier AJ – Clinical Social Worker
AJ is used for services delivered by Licensed Clinical Social Workers. LCSWs play a major role in therapy and care coordination, especially in community and outpatient settings. Medicaid plans often require AJ to distinguish LCSWs from other therapist types.
Modifier HO – Master’s Level Provider
HO applies to clinicians with a master’s degree, such as LPCs, LMFTs, and LMHCs. Many therapy services are reimbursed under this modifier, but often at a different rate than doctoral-level providers. Misusing HO can lead to underpayment or claim rejection.
Modifier HP – Doctoral Level Provider
HP is used for PhD- or PsyD-level clinicians. This modifier supports higher reimbursement and broader CPT eligibility in many payer contracts. It is commonly required for advanced diagnostic and psychological testing services.
Modifier HN – Bachelor’s Level Provider
HN is primarily used in Medicaid programs for bachelor-level clinicians working under supervision. Coverage is limited, and documentation requirements are strict. Claims with HN must clearly show supervision and program eligibility.
These license modifiers directly affect payment amounts, CPT eligibility, and audit risk. One wrong modifier can undo an otherwise clean claim.
Program and Setting Modifiers
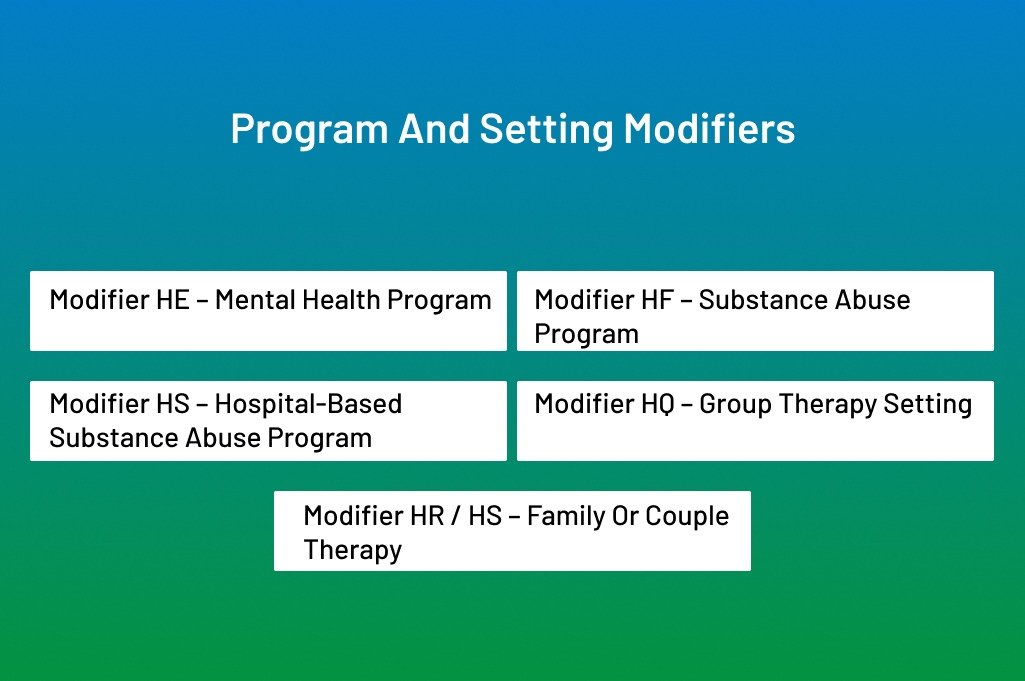
Behavioral health services are often delivered within structured programs rather than simple office visits. Program and setting modifiers tell payers where and under what model care was provided.
These modifiers matter because many CPT codes are reimbursed only when tied to an approved program type.
Modifier HE – Mental Health Program
HE indicates that services were provided under a designated mental health treatment program. This modifier is standard in community mental health centers and Medicaid-funded services.
Modifier HF – Substance Abuse Program
HF applies to services delivered as part of a substance use disorder treatment program. It helps payers separate behavioral health therapy from general mental health care.
Modifier HS – Hospital-Based Substance Abuse Program
HS is more specific. It identifies substance abuse services delivered within a hospital-based program. This distinction affects reimbursement and reporting.
Modifier HQ – Group Therapy Setting
HQ signals that the service was provided in a group setting. This modifier is essential when billing group psychotherapy codes. Missing HQ often results in bundling denials.
Modifier HR / HS – Family or Couple Therapy
These modifiers clarify when therapy involves family members or couples rather than individual treatment. They support medical necessity and correct CPT pairing.
Even with the correct CPT code, using the wrong program or setting modifier can cause a claim to be rejected instantly.
Modifiers That Support Medical Necessity
Some modifiers do more than explain logistics. They tell the payer that special coverage rules have been met.
Modifier KX
KX confirms that the service meets the payer’s medical necessity requirements. It is commonly required when therapy exceeds annual visit limits, time thresholds, or frequency caps.
KX should never be added casually. When auditors see this modifier, they expect strong documentation. Treatment plans, progress notes, and clinical justification must align perfectly.
Used correctly, KX keeps extended care eligible for reimbursement. Used carelessly, it invites audits.
Modifier 52 – Reduced Services
Not every session runs its full course. Modifier 52 accounts for that reality.
This modifier is used when a service is partially reduced but still medically necessary and billable. In behavioral health, this often happens due to patient distress, early termination, safety concerns, or unavoidable technical disruptions.
The key is documentation. The record must clearly explain why the session ended early and what portion of the service was completed. Without that explanation, payers may deny the claim or request a refund later.
Common Modifier Mistakes in Behavioral Health and How to Avoid Them
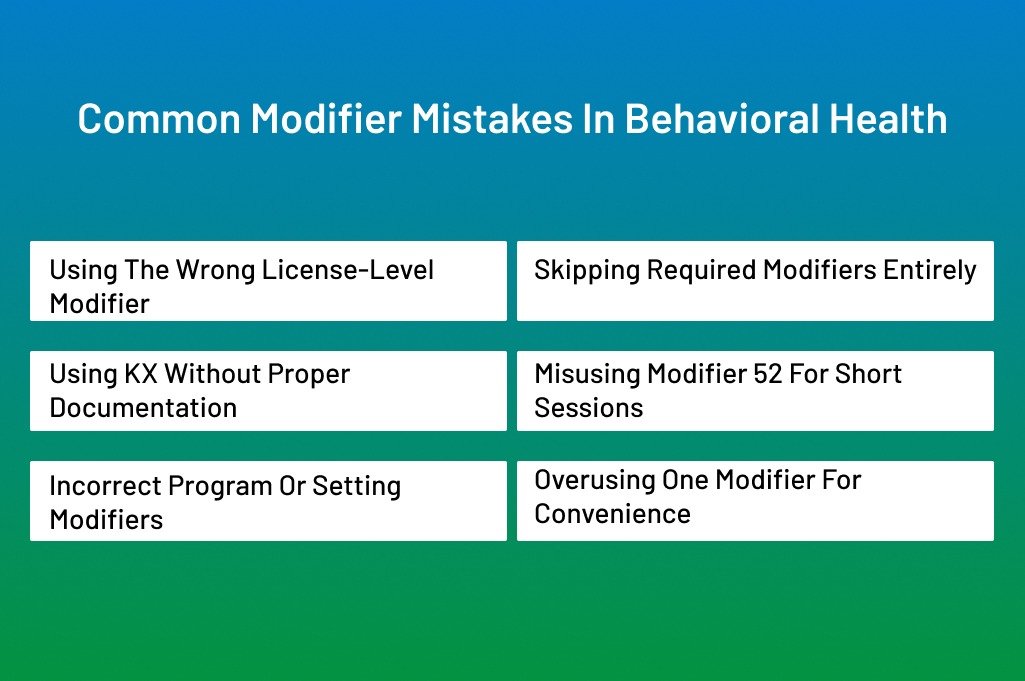
In behavioral health billing, modifiers are small details with big consequences. One wrong modifier can turn a clean claim into a denial, delay payment for weeks, or trigger an audit. Many practices do solid clinical work but lose revenue because modifiers are applied out of habit rather than as part of a strategy. Let’s break down the most common mistakes and how to stay clear of them.
Using the Wrong License-Level Modifier
This is one of the most frequent and costly errors. Practices often apply the same modifier to every clinician, even when credentials differ.
For example, billing all therapy services with modifier HO even when a PsyD or PhD delivered the session, and/or using AH for a provider who is actually an LCSW. Payers rely on these modifiers to decide eligibility and rates. When the modifier does not match the provider’s license on file, the claim often gets denied or paid at a lower rate.
How to avoid it: Keep an updated provider credential matrix. Link each clinician’s license, degree, and payer enrollment to the correct modifier inside your billing system—train staff to verify the rendering provider before submitting claims.
Skipping Required Modifiers Entirely
Some claims fail not because the modifier is wrong, but because it is missing. Medicaid plans are especially strict about this.
A typical example is billing therapy without a license-level modifier, assuming the NPI alone is enough. Another is forgetting HQ for group therapy or HE for program-based services. Without these signals, payers cannot process the claim correctly.
How to avoid it: Create payer-specific modifier checklists. Before submission, confirm that every required modifier is present. Think of modifiers as part of the CPT code, not optional add-ons.
Using KX Without Proper Documentation
Modifier KX is powerful, but risky. Many practices use it to push claims past visit limits without realizing it flags the claim for scrutiny.
If the documentation does not clearly support medical necessity, payers may deny the claim retroactively or demand refunds months later. This is where many audits begin.
How to avoid it: Only use KX when the treatment plan, progress notes, and clinical rationale clearly justify extended care. Make sure documentation answers the question: why does this patient need more services now?
Misusing Modifier 52 for Short Sessions
Modifier 52 is often misunderstood. Some practices apply it automatically when a session runs short, even if the payer does not allow reduced billing for that CPT code.
Other times, the modifier is used, but the reason for the shortened session is missing from the note. This leaves the claim vulnerable during review.
How to avoid it: Check payer policies before using modifier 52. Document exactly why the service was reduced and what portion was completed. If it is not documented, it did not happen.
Incorrect Program or Setting Modifiers
Behavioral health services often depend on where and how care is delivered. Using HF instead of HE, or omitting HS for hospital-based programs, can cause claims to be rejected even when the CPT code is correct.
This mistake usually happens when staff reuse old claim templates without adjusting them for the setting.
How to avoid it: Tie the program and setting modifiers to locations or service lines in your billing software. Review claims whenever services move between offices, hospitals, or structured programs.
Overusing One Modifier for Convenience
Some practices rely too heavily on one modifier because “it usually works.” This might get claims paid in the short term, but it creates long-term compliance risks.
Payers notice patterns. If every claim uses the same modifier regardless of provider or setting, audits are sure to follow.
How to avoid it: Match modifiers to reality, not convenience. Review modifier usage reports regularly to spot patterns that look too uniform.
Conclusion
Modifiers may be just two characters, but in behavioral health billing, they carry significant weight. Using the wrong modifier—or skipping one—can lead to denials, delayed payments, or lost revenue. By understanding license-level, program, telehealth, and medical-necessity modifiers, providers can ensure that claims accurately reflect the services delivered.
The key is consistency: verify provider credentials, match modifiers to the service and setting, and support every modifier with proper documentation. Regular staff training, thorough audits, and updated payer guidelines keep your billing clean and compliant.
When applied correctly, modifiers not only protect your revenue but also streamline claims, reduce denials, and maintain a transparent, professional relationship with payers. In short, mastering modifiers is mastering the path to accurate reimbursement and a healthier revenue cycle.
Take the Stress Out of Mental Health Billing
Behavioral health billing is complex. License-level modifiers, telehealth rules, Medicaid requirements, supervision guidelines — one small mistake can delay payment or trigger denials.
At ANR Medical Billing, we provide end-to-end mental health billing services designed specifically for therapy practices, psychiatrists, psychologists, LCSWs, and community mental health programs.
We handle:
- CPT & modifier accuracy
- Telehealth billing compliance
- Medicaid and Medicare behavioral health billing
- Prior authorizations
- Claims submission and denial management
- A/R follow-up and revenue optimization
You focus on patient care. We’ll handle the revenue cycle.
Request a Free Billing Assessment Today and See Where Revenue Is Being Lost.
