Durable Medical Equipment billing looks straightforward at first glance. Pick a code. Submit a claim. Get paid.
But anyone who has worked hands-on with DME claims knows it rarely works that way.
HCPCS codes sit at the center of every DME transaction. They decide how equipment is classified, how it is billed, and whether reimbursement moves forward or gets stuck in review.
A single coding, documentation, or modifier mistake can delay payment for months or trigger audits that no practice wants to deal with. Many providers rely on specialized DME billing services to prevent these issues before claims are submitted.
This guide breaks down HCPCS codes for DME in a way that mirrors how billing actually happens.
From understanding what qualifies as DME to navigating Medicare rules, documentation standards, and reimbursement workflows, the goal is simple: to provide a comprehensive guide. Help you submit cleaner claims, reduce denials, and protect your revenue.
Whether you are a provider, DME supplier, or billing manager, this guide gives you clarity where most billing resources fall short.
What Is DMEPOS in HCPCS Billing?
Medicare does not classify billing simply as DME. It uses the broader category known as DMEPOS — Durable Medical Equipment, Prosthetics, Orthotics, and Supplies.
This terminology is used by the Centers for Medicare & Medicaid Services (CMS) and appears in:
- Fee schedules
- Coverage determinations
- Prior authorization lists
- Audit documentation
Using the term DMEPOS strengthens semantic alignment with Medicare policy language and increases topical relevance for federal search intent.
HCPCS in DME Billing
Before diving into billing rules, it helps to understand what HCPCS codes actually are and why DME relies on them so heavily.
HCPCS stands for Healthcare Common Procedure Coding System. While CPT codes describe physician services and procedures, HCPCS Level II codes describe supplies, DME, prosthetics, orthotics, and non-physician items.
DME billing lives almost entirely in the HCPCS Level II world.
Medicare requires HCPCS Level II codes for all DMEPOS claims. Most commercial payers follow Medicare’s lead, even when they apply their own coverage policies.
In short, if you bill DME in the U.S., HCPCS codes are non-negotiable.
What Qualifies as Durable Medical Equipment (DME)?
Not every medical item qualifies as DME, even if it sounds like one. Medicare uses precise criteria.
To be considered DME, the item must:
- Withstand repeated use
- It is primarily used for a medical purpose
- Not be helpful to someone without illness or injury
- Be appropriate for use in the home
That last point matters more than most people realize. If equipment is used only in a facility setting, Medicare usually does not classify it as DME.
Examples of common DME include wheelchairs, walkers, oxygen equipment, CPAP machines, hospital beds, and patient lifts.
Supplies like catheters or diabetic test strips may still use HCPCS codes, but they fall under DMEPOS, not always strict DME.
Structure of HCPCS Level II Codes for DME
HCPCS Level II codes follow a predictable format. They always start with a letter, followed by four numbers.
For DME, most codes fall into these letter ranges:
- E codes – Durable medical equipment (wheelchairs, hospital beds, oxygen equipment)
- K codes – Temporary DME codes
- L codes – Orthotics and prosthetics
- A codes – Medical supplies
- B codes – Enteral and parenteral therapy
Understanding the letter category helps you spot errors early. If a wheelchair is coded with an A code, something is wrong.
Common HCPCS DME Code Categories
Mobility Equipment Codes
Mobility equipment makes up a large share of DME claims. These codes fall mainly under E codes.
Manual wheelchairs, power wheelchairs, scooters, walkers, and accessories each have separate codes. Medicare closely scrutinizes medical necessity here.
For example, a power wheelchair is not covered just because a patient prefers it. Documentation must show that the lesser equipment will not meet the patient’s needs.
Even accessories like cushions or leg rests require separate HCPCS codes and justification.
Hospital Beds and Accessories
Hospital bed codes also fall under E codes. Coverage depends heavily on the patient’s condition.
Adjustable beds are not automatically covered. Documentation must support conditions such as severe arthritis, spinal injury, or positioning needs.
Accessories like trapeze bars or side rails must be billed separately and justified in the medical record.
Oxygen and Respiratory Equipment
Oxygen equipment billing is one of the most regulated areas in DME.
Codes cover oxygen concentrators, portable oxygen, oxygen contents, and accessories. Medicare requires:
- Blood gas or oximetry testing
- Detailed physician orders
- Continued need for documentation
Rental rules apply here, and payments are often spread over multiple months rather than a single lump sum.
CPAP and Sleep Therapy Equipment
CPAP devices are assigned specific E codes and are subject to strict compliance rules.
Medicare requires proof that the patient actually uses the device. Usage data often must show a minimum number of hours per night over a defined period.
Failure to submit compliance documentation can result in recoupments, even after initial payments.
The DME Billing Process Using HCPCS Codes
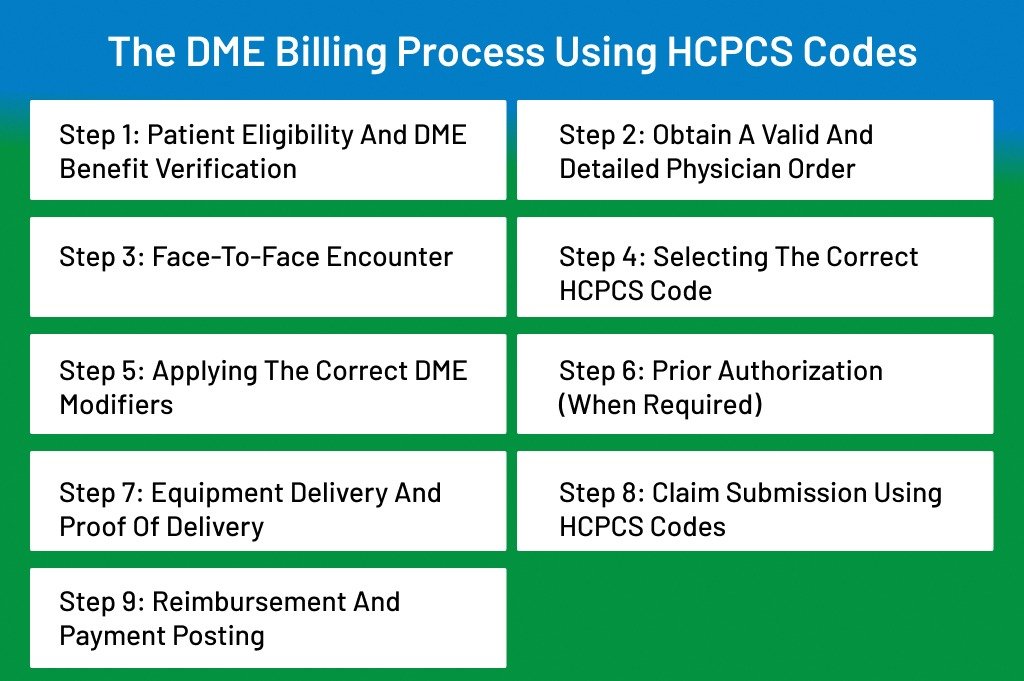
DME billing does not fail because of one big mistake.
It usually breaks down because of small gaps at each step.
- A missing modifier.
- An unsigned order.
- Eligibility was checked too late.
When those gaps add up, claims stall, denials pile up, and cash flow slows down.
The DME billing process using HCPCS codes follows a strict sequence. Every step builds on the previous one. If one step is weak, the entire claim becomes vulnerable.
Let’s walk through the whole process the way it actually works in U.S. healthcare.
Step 1: Patient Eligibility and DME Benefit Verification
Everything starts here. Not after delivery. Not after coding.
Right here.
Before assigning any HCPCS code, you must confirm that the patient actually has DME coverage.
Medicare Part B covers most DME, but even Medicare has conditions, rental rules, and frequency limits. Medicare Advantage plans add another layer with prior authorization and network restrictions. Commercial payers vary even more.
Eligibility verification should confirm:
- Active coverage on the date of service
- DME benefit availability
- Rental vs purchase rules
- Prior authorization requirements
- Patient responsibility (deductible, coinsurance)
Skipping this step is like driving with your eyes closed. You may move forward, but the crash comes later.
Step 2: Obtain a Valid and Detailed Physician Order
HCPCS codes alone do not justify payment.
The order does.
DME requires a written order before delivery (WOPD) for many items, especially Medicare claims. The order must be specific. Generic wording leads to denials.
A valid order should clearly include:
- Patient name
- Order date
- Detailed description of the equipment
- Length of need
- Treating provider signature
If the HCPCS code describes a power wheelchair, the order must reflect that level of detail. “Wheelchair as needed” is not enough.
Think of the order as the legal foundation of the claim.
Step 3: Face-to-Face Encounter and Medical Necessity Documentation
This is where many DME claims quietly die.
Medicare requires a face-to-face encounter for several DME categories. The provider must document why the equipment is medically necessary.
Good documentation tells a story.
It explains:
- The patient’s condition
- Functional limitations
- Why is the equipment required in the home
- Why simpler alternatives will not work
If you code a hospital bed HCPCS code, the notes must justify the need for positioning or medical conditions requiring it.
HCPCS codes describe equipment. Documentation proves the need.
Proper documentation review is a core part of our medical billing services, ensuring claims meet Medicare standards before submission.
Step 4: Selecting the Correct HCPCS Code
Now coding comes into play.
Choosing the correct HCPCS Level II code means matching the exact item provided to the official code description. Close is not good enough.
DME HCPCS codes differ by:
- Equipment type
- Level of complexity
- Accessories
- Usage method
Even small differences matter. A standard walker and a rolling walker use different HCPCS codes. Billing the wrong one invites audits.
Always use the most current HCPCS code set. Deleted or outdated codes result in automatic rejections.
Step 5: Applying the Correct DME Modifiers
Modifiers are not optional in DME billing.
They explain how the equipment is provided.
Common DME modifiers include:
- NU for new equipment
- RR for rental
- UE for used equipment
- KX to confirm coverage criteria are met
Without the correct modifier, the payer cannot process the claim correctly. Many DME claims deny simply because the modifier is missing or mismatched.
Think of modifiers as instructions to the payer’s system.
Incorrect modifier usage is one of the leading causes of DME insurance claim denials — something experienced revenue cycle management services help prevent.
Step 6: Prior Authorization (When Required)
Some HCPCS codes trigger mandatory prior authorization, especially under Medicare and Medicare Advantage plans.
High-risk DME items such as power mobility devices often fall under this rule.
Prior authorization confirms coverage before delivery. Submitting claims without it usually guarantees denial.
Documentation submitted for authorization should mirror what will later support the claim. Any mismatch raises red flags.
Step 7: Equipment Delivery and Proof of Delivery
No proof of delivery, no payment.
It is that simple.
Proof of delivery (POD) must show:
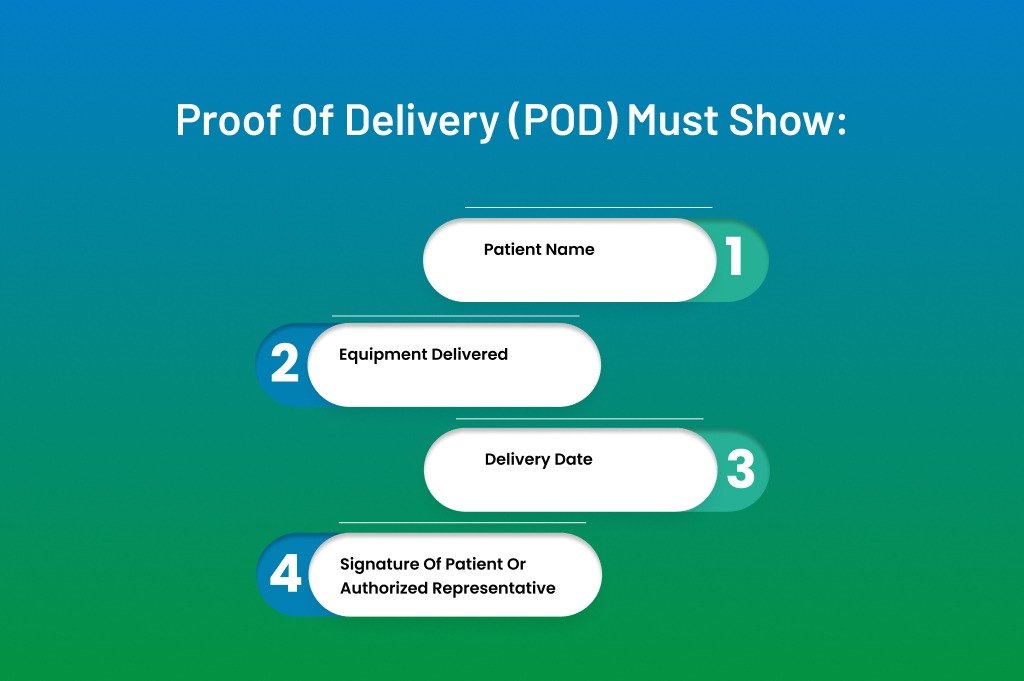
- Patient name
- Equipment delivered
- Delivery date
- Signature of patient or authorized representative
For shipping, tracking confirmation may be required. For in-person delivery, a signed acknowledgment is critical.
The delivery date often determines the billing date, especially for rentals.
Step 8: Claim Submission Using HCPCS Codes
Once all documentation is complete, the claim can be submitted.
DME claims are usually submitted on the CMS-1500 or its electronic equivalent. The claim must include:
- Correct HCPCS code
- Proper modifiers
- Units of service
- Place of service
- Ordering provider details
Accuracy here matters. Even minor errors can push claims into manual review.
Step 9: Reimbursement and Payment Posting
DME reimbursement rarely comes instantly.
Medicare pays based on the DME fee schedule, which varies by geographic area. Many items are paid for as monthly rentals rather than one-time purchases.
Payments should be posted carefully. Partial payments often indicate rental billing or capped rental schedules.
Always reconcile payments against expected allowed amounts.
Medicare DME Fee Schedule and Competitive Bidding
Medicare reimburses DME using the DMEPOS fee schedule published annually by CMS. Rates vary by geographic region and competitive bidding adjustments.
Suppliers must verify:
- Fee schedule region
- Competitive bidding applicability
- Capped rental status
- Purchase vs rental category
Failure to align billing with the correct fee schedule amount can result in underpayments or recoupments.
Medicare Administrative Contractors (DME MACs)
Medicare DME claims are processed through regional DME Medicare Administrative Contractors (DME MACs). These contractors interpret Local Coverage Determinations (LCDs) and apply policy rules to HCPCS-coded claims.
Suppliers must align documentation with:
- Local Coverage Determinations (LCDs)
- National Coverage Determinations (NCDs)
- DME MAC policy articles
Failure to meet LCD criteria is one of the leading causes of DME denials.
Conclusion
HCPCS coding for DME is not just a technical task. It is a compliance responsibility, a revenue driver, and often the deciding factor between smooth reimbursement and repeated denials.
Every step in the DME billing process matters. Eligibility checks set expectations. Physician orders establish legal support. Documentation proves medical necessity. HCPCS codes and modifiers translate care into payable claims. Miss one piece, and the entire claim weakens.
Medicare and commercial payers continue to tighten oversight around DME. Audits are more frequent. Documentation standards are higher. Suppliers and practices that rely on guesswork or outdated workflows feel the impact quickly.
That is why experienced billing support makes a real difference.
Struggling With HCPCS Codes for DME?
DME billing is one of the most audited areas in healthcare. ANR Medical Billing specializes in durable medical equipment billing services designed to reduce denials, strengthen compliance, and maximize Medicare reimbursement.
From HCPCS code accuracy and modifier validation to prior authorization management and denial appeals, our team protects your revenue at every stage of the DMEPOS billing process.
If your DME claims are slowing cash flow or increasing audit exposure, now is the time to optimize your workflow.
Partner with ANR Medical Billing and turn complex DME billing into predictable, compliant revenue.
Frequently Asked Questions About HCPCS Codes for DME
What are HCPCS Level II codes used for in DME billing?
They describe durable medical equipment, supplies, prosthetics, and orthotics used in DMEPOS claims.
Does Medicare require prior authorization for all DME?
No. Only certain high-risk HCPCS codes require mandatory prior authorization.
What modifier is used for DME rental billing?
Modifier RR indicates rental equipment.
What is DMEPOS in Medicare billing?
DMEPOS stands for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies.
