If you’ve ever run a therapy practice — or even one solo office with a tight schedule and too many patients — you already know the love–hate relationship clinicians have with CPT 90837.
On one hand, it reflects a full, meaningful therapy hour. On the other hand, it attracts payer scrutiny like a magnet.
Therapists want to use it. Insurance companies want you to “justify” using it.
Auditors? They keep it pinned right at the top of their “Let’s double-check this provider” list.
But here’s the good news:
When you understand exactly when 90837 is appropriate, how to document it cleanly, and how to bill it without triggering denials, this code becomes one of the most reliable revenue boosters in behavioral health.
What is CPT Code 90837?
CPT 90837 is the code for a full 60-minute psychotherapy session.
It’s the “deep work” therapy hour — the kind of session where a therapist and client spend 53–60 minutes on real clinical treatment, not just casual conversation.
When someone bills 90837, it means the session included structured, skill-based therapy such as CBT, EMDR, DBT, ACT, trauma processing, emotional regulation work, or symptom assessment. It also means the therapist guided the session toward actual treatment goals—checking safety, exploring patterns, and adjusting the plan as needed.
It doesn’t cover things like medication management, paperwork, casual conversation, or coaching. Insurance pays for 90837 only when real psychotherapy happens for a full clinical hour.
In simple terms:
90837 = an actual 60-minute therapy session with meaningful clinical work, not just time spent talking.
Who Is Allowed to Bill 90837?
Only licensed mental health professionals with a psychotherapy scope can bill it:
- Psychologists
- Psychiatrists
- LICSW / LCSW
- LPC / LPCC
- LMFT
- Psychiatric NPs & PAs (when providing therapy)
- Clinical nurse specialists in mental health
Unlicensed interns, wellness coaches, and peer supporters are out unless they are payer-approved and supervised.
When 90837 Is Clinically Appropriate?
You don’t bill a 60-minute session because you want to — you bill it because the clinical picture demands it.
Below are real situations where 90837 makes sense:
Trauma Work That Needs Uninterrupted Time
EMDR, prolonged exposure, or trauma-focused CBT often reaches the full hour.
Stopping midway can destabilize the patient.
Complex Diagnoses With High Symptom Severity
People with severe depression, PTSD, bipolar disorder, OCD, panic attacks, or eating disorders often need extended time for emotional unpacking.
Multiple Stressors in a Single Visit
Like: breakup + job loss + insomnia + relapse triggers = an hour, easily.
Intense Family Dynamics Sessions
When you involve parents, spouses, or caregivers — and you’re still providing psychotherapy — the time stretches.
High-Risk Patients
Suicidal ideation, self-harm urges, dissociation episodes — these require more than a quick check-in.
Sessions With Many Interventions
You’re using grounding, restructuring, psychoeducation, and safety planning all in the same session. That’s a full hour of work.
2025 Reimbursement for CPT 90837
The payout for a 90837 session in 2025 depends heavily on the payer, and the differences can feel dramatic. Some payers value the clinical hour properly, while others.. well, not so much. Here’s how the numbers realistically shake out across the industry:
Typical 2025 Reimbursement Ranges
- Medicare: $125 – $145: Reliable and predictable, sitting comfortably in the mid-range.
- Medicaid: $60–$95. Consistently the lowest payer, which won’t surprise any therapist.
- Commercial Insurance: $110 – $210: The widest range and usually the highest-paying category.
- Cash Pay: $150–$275. Private-pay clients often reflect the actual market value of a full clinical hour.
Overall, commercial plans and cash-pay sessions tend to provide the strongest reimbursement, while Medicaid stays at the bottom of the scale. The gap between payers can be frustrating, but it’s the reality most practices see heading into 2025.
Documentation Requirements for Code for 90837
To get smooth payments, your note must quietly answer a payer’s unspoken questions:
What did you do for 60 minutes?
You need psychotherapy content, not diary entries.
Include:
- What symptoms were addressed
- What interventions did you use
- Patient’s response
- Any breakthroughs or setbacks
- Clinical observations
- Progress toward goals
Why did the session require the whole hour?
Insurance wants justification—brief but clear.
Examples:
- “Session required extended trauma processing.”
- “Multiple crises addressed simultaneously.”
- “Severe anxiety with dissociation required prolonged grounding.”
Exact timing
Write it cleanly:
“Session: 2:30 PM – 3:30 PM (60 minutes psychotherapy)”
Safety assessment
For long sessions, include at least one line:
“Patient denies SI/HI.”
(or document concerns when present)
Telehealth requirements (if applicable)
Add:
- Patient location
- Provider location
- Consent
- Platform used
Something like:
“Telehealth session conducted with consent via secure video platform; patient located at home.”
How to Bill CPT 90837 (Step-by-Step)
Billing 90837 isn’t complicated once you understand its rhythm. It’s like a checklist you follow every time you deliver a full clinical hour. The cleaner your steps, the cleaner your reimbursement — and the fewer letters you get from Insurance asking, “Can you please explain why this session took so long?”
Here’s how you can bill this code accurately:
Make Sure the Session Actually Hits 53–60 Minutes
Insurance cares about clinical minutes, not calendar minutes.
If it’s 52 minutes or less, switch to 90834.
Let your EHR automatically add timestamps so you never have to think about it.
Verify Benefits Before the First Appointment
Even if the patient swears they’re “fully covered,” check anyway.
Your verification should confirm:
- Does their plan cover 90837?
- Do they need preauthorization?
- What is the copay or coinsurance?
- Are there visit limits?
- Is the provider in-network or out-of-network?
A 2-minute phone call saves hours of denials later.
Document the Session Like a Clinician — Not a Novelist
Insurance wants clinical clarity, not a diary entry.
Your note should quietly answer:
- What symptoms did you address?
- What interventions did you use? (CBT, EMDR, DBT, etc.)
- Why did the session require the whole hour?
- How did the client respond?
- Any risks or safety assessments?
- Exact start/end time.
This is the backbone of getting paid.
Add Telehealth Details (If Online)
Missing this is one of the most common reasons for denial.
Include:
- Consent
- Patient location
- Provider location
- Platform used
Example: “Telehealth session conducted via secure video platform with patient’s consent; patient located at home.”
Submit the Claim With the Correct Details
Your claim should include:
- CPT code: 90837
- Diagnosis code(s): ICD-10
- Place of service (e.g., 11 for office, 10 for telehealth)
- NPI and Tax ID
- Payer ID
- Exact session date
Small typos cause big delays.
Attach Authorization Numbers if Required
Some commercial plans require preauthorization for 90837.
If so, add the auth number directly on the claim.
No auth = instant denial.
Track the Claim Until It Gets Paid
Don’t assume “submitted” means “covered.”
Monitor:
- Has the payer received it?
- Was it processed?
- Was it denied or partially paid?
- Is a correction or appeal needed?
Behavioral health claims are denied more often than medical claims — so consistent follow-up is money in the bank.
Appeal Every Incorrect Denial
90837 denials get overturned a lot when notes are solid.
Appeal if they say:
- “Time not justified”
- “Not medically necessary”
- “Insufficient documentation”
One clean appeal letter with your note attached usually does the trick.
Collect Patient Responsibility Promptly
Copays, deductibles, and coinsurance add up—Bill patients quickly so you don’t lose revenue to delay or forgetfulness.
Common 90837 Billing Mistakes — And How to Fix Them?
Therapists don’t mess up because they don’t care. They mess up because billing rules feel like someone mixed tax law with alphabet soup. Here are the most common 90837 mistakes and the simple fixes that keep your claims clean and audit-proof.
Billing 90837 for a 45-Minute Session
Sometimes the session feels like an hour because everyone was emotionally exhausted — but Insurance only cares about the clock.
Fix:
- Write the exact start and end times.
- If the session is under 53 minutes, bill 90834, not 90837.
Copy-Paste Notes That Look the Same
If twenty notes in a row use the same sentence (“Patient engaged well. CBT used.”), Insurance sees a red flag instantly.
Fix:
- Add just one or two unique sentences each time.
- It shows the session was real and clinically meaningful.
No Clinical Reason for the Extended Time
“Patient needed the full session” isn’t enough. Insurers want the why behind the longer service.
Fix — Add the clinical reason:
- Trauma processing
- Multiple acute issues
- Crisis de-escalation
- Intensive cognitive restructuring
Even a short explanation does the job.
Using 90837 for Every Session
If 90–95% of your sessions are coded as 90837, you’re an instant audit target.
Fix:
- Use 90834 for shorter or lighter sessions.
- Only use 90837 when clinically justified.
Missing Telehealth Details
Telehealth denials often come from tiny missing details like consent or location.
Fix
- Client consented to telehealth
- Client location
- Platform used (Zoom, Doxy, etc.)
That’s all Insurance needs to see.
Mixing Medication Management Into the Time
If you review meds during the session, it counts as a split service—not a pure psychotherapy hour.
Fix:
- Keep the time separate
- Med management = E/M code
- Therapy = psychotherapy code
- Combined example: 99214 + 90836
Not Documenting Safety Checks
Longer sessions often explore heavy emotional topics, so documenting safety is essential.
Fix:
- Add one simple sentence showing that safety was assessed.
- It protects the client and your claim.
Pro Tips to Maximize 90837 Payments Without Extra Stress
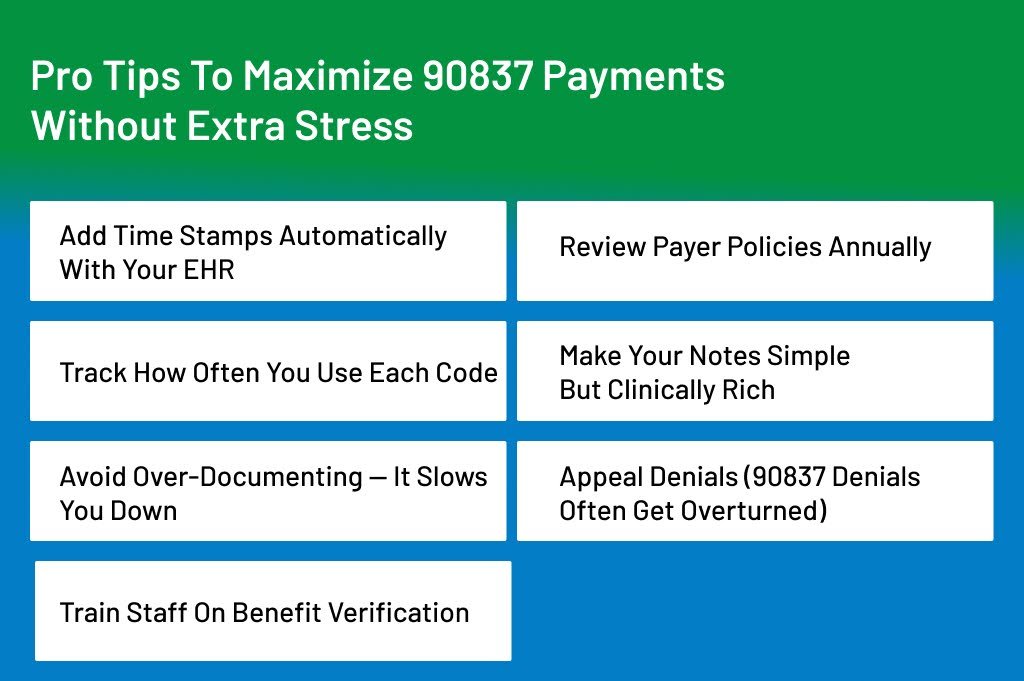
Use these, and your revenue will stabilize fast:
- Add time stamps automatically with your EHR
- Review payer policies annually
- Track how often you use each code
- Make your notes simple but clinically rich
- Avoid over-documenting — it slows you down
- Appeal denials (90837 denials often get overturned)
- Train staff on benefit verification
Conclusion
CPT 90837 can feel like both a blessing and a headache. It’s the code that represents the most meaningful therapy work—those deep, structured, clinically focused sessions that actually move patients forward. But it also attracts the most scrutiny, which is why so many therapists get nervous every time they hit “submit claim.”
The real win comes when you understand precisely how to use it, document it, and defend it.
Once you get comfortable showing why the whole hour was clinically necessary, 90837 becomes one of the strongest, most predictable revenue generators in your practice.
It rewards careful documentation, clear clinical reasoning, and honest time tracking. And when you follow the rules, you get paid faster, avoid denials, and stay far away from payer audits.
If you’re stepping into 2025 aiming for smoother billing days, fewer headaches, and more reliable reimbursements, mastering 90837 is absolutely worth the effort. The code isn’t your enemy—it’s misunderstood.
Use it the right way, back it up with clean notes, and you’ll see the difference in both patient outcomes and monthly revenue.
Let ANR Billing Handle 90837 So You Can Focus on Patients
If you’re tired of fighting with payers, second-guessing documentation rules, or losing money to preventable 90837 denials, ANR Billing can take the entire burden off your shoulders. We specialize in behavioral health billing and know precisely how to protect your revenue from coding errors, audits, and slow-paying insurance plans.
Here’s what we do for you:
- Clean claim submissions with proper time-based coding
- Payer-specific documentation checks for 90837
- Denial management and aggressive appeals
- Behavioral health–trained billers who know your workflows
- Transparent reporting, faster reimbursements, and zero guesswork
You deliver the clinical hour.
We ensure you get paid accurately and on time.
Struggling With CPT 90837 Denials or Documentation Issues?
ANR Medical Billing specializes in psychiatry and behavioral health billing, helping therapists accurately code 60-minute sessions, reduce audit risk, and receive payment faster.
👉 Get Expert Psychiatry Billing Services from ANR Medical Billing
