There are a handful of CPT codes that every mental health provider must understand on Day 1, and 90791 sits at the very top of that list. It’s the code you use when a patient first walks through your door and says, “Something’s wrong, and I need help.”
Think of it as the foundation of the patient’s entire mental health journey. If you code it correctly, document it clearly, and bill it according to payer rules, everything that follows becomes easier—from treatment planning to claims approval. But if you mess up 90791, the entire case can wobble like a chair missing a screw.
Let’s walk through everything you need to know about CPT Code 90791.
What Is CPT Code 90791?
The CPT code 90791 is used for a complete psychiatric diagnostic evaluation — without medical services.
That means you’re performing a non-medical mental health intake where you:
- Study the patient’s symptoms
- Explore history (psych, medical, family, social)
- Conduct a complete Mental Status Exam
- Assess risk factors
- Form a diagnostic impression
- Build a treatment plan
You’re doing all the thinking but not prescribing meds or providing medical procedures.
This code is used for:
- New patients
- Returning patients with a brand-new issue
- Patients whose condition changed enough to require a complete re-evaluation
If you add a medication evaluation or change medication?
That’s 90792, not 90791.
Who Can Bill CPT 90791?
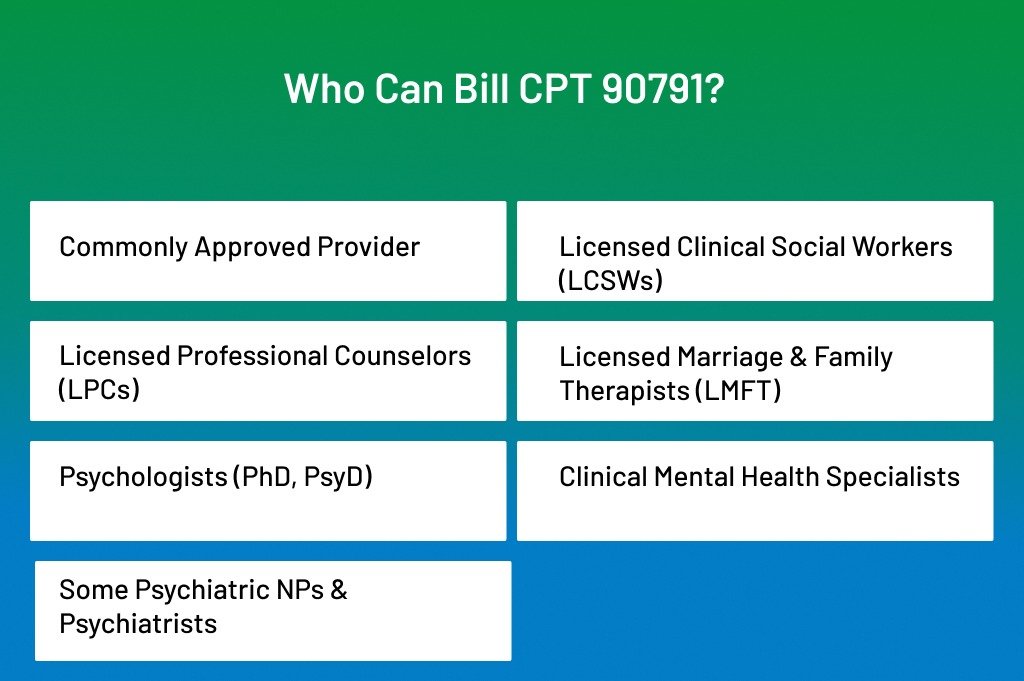
This part always feels like sorting laundry in the dark — every state, every insurer, and sometimes every plan inside the same insurer has its own rulebook. But let’s clear the fog and walk through the general standards most payers follow.
- Commonly Approved Providers: These clinicians almost always qualify because they hold independent mental-health licensure and provide diagnostic evaluations as part of their scope of practice.
- Licensed Clinical Social Workers (LCSWs): LCSWs typically conduct the bulk of intake assessments in outpatient settings. Insurers treat their diagnostic work as fully billable under 90791.
- Licensed Professional Counselors (LPCs): Most commercial payers accept LPCs for 90791 because intake evaluations fall squarely into their clinical responsibilities.
- Licensed Marriage & Family Therapists (LMFT): Family-focused clinicians can use 90791 when the evaluation centers on mental-health assessment, diagnostic formulation, or treatment planning.
- Psychologists (PhD, PsyD): These are the gold standard for diagnostic evaluations. Nearly every payer recognizes them for 90791 without hesitation.
- Clinical Mental Health Specialists: This includes licensed mental-health clinicians whose state boards authorize them to perform diagnostic evaluations.
- Some Psychiatric NPs & Psychiatrists (only if no medical component is included): Here’s where it gets tricky. If the provider performs a purely psychological evaluation without reviewing meds, ordering labs, or doing a medical exam, then 90791 may apply. But if any medical services enter the mix, jump to 90792 instead.
Who Usually Cannot bill 90791
Some clinicians run into walls not because of skill, but because of payer or licensure limitations.
- Pre-licensed associates or interns: Titles such as AMFT, APC, LMSW, MFT-I, and similar often come with restrictions. Some payers allow them to bill under supervision, but many don’t. Always check the plan contract.
- Coaches, caseworkers, peer support specialists, or anyone without a mental-health license: Even if they provide intake-like services within an agency, insurance considers them unqualified to perform diagnostic evaluations. No recognized license = no 90791.
When Should You Use 90791?
Think of 90791 as the “full clinical reset button.” Anytime you need to step back, gather the whole picture, and re-evaluate the patient’s mental health status, this is your code.
- First-ever appointment: the classic use case: a new patient, a new chart, a new clinical story.
- When a patient switches providers within the same practice: If you’re inheriting the case, you’ll want to reassess symptoms, risks, history, diagnosis — basically everything.
- After a major clinical shift: A relapse, traumatic event, significant mood shift, or new symptoms usually justify a fresh, comprehensive assessment.
- When restarting treatment after a long break (typically 6+ months), Most payers allow a new 90791 when the clinical picture has aged enough that you genuinely need a new baseline.
When NOT to Use 90791
If the visit isn’t a complete clinical evaluation, you’ll want a different code.
- For ongoing weekly or biweekly therapy, those sessions fall under psychotherapy codes usually 90834 or 90837, depending on the duration.
- When performing medication-related work: If you’re reviewing meds, adjusting doses, or completing a medical evaluation, use 90792 instead.
- For quick, problem-focused check-ins: If you’re not performing a head-to-toe diagnostic assessment, 90791 doesn’t fit.
Billing and Coding Guidelines for CPT Code 90791
Before you can bill 90791 confidently, you need to understand how payers interpret it, what documentation they expect, and how to code it without raising red flags. Many clinicians think of 90791 as “just the intake.” Still, insurance companies see it as a high-value diagnostic service — which means they want proof that you completed a full evaluation and not just an extended therapy session.
Understand What 90791 Actually Represents
Insurance sees 90791 as a complete psychiatric diagnostic evaluation without medical services. That means you’re gathering the complete clinical picture — symptoms, history, functioning, risks, and diagnostic impressions — but not prescribing or adjusting medications.
If you include med management, the code automatically jumps to 90792, so keep the boundary clear.
Make Sure the Visit Qualifies for 90791
Not every “first visit” qualifies. To bill 90791 legitimately, the session must include all the core components of a diagnostic evaluation:
- Comprehensive symptom review
- Mental Status Exam
- Psychosocial, medical, and family history
- Risk assessment (SI/HI, self-harm, violence, substance use)
- Diagnostic formulation
- Treatment plan development
If your evaluation is brief, problem-focused, or missing major components, insurers expect you to use a different code.
Use 90791 when:
- You’re establishing care with a new patient
- A patient transfers from another provider
- There’s a significant change in condition
- A long gap in treatment requires a fresh assessment
Don’t use 90791 when:
- The visit is strictly psychotherapy
- You’re only checking progress
- You’re prescribing or adjusting medication (90792)
Use Accurate Provider Credentials
90791 has different coverage rules depending on the payer.
Most insurers allow:
- LCSW
- LPC / LPCC
- LMFT
- Psychologists (PhD/PsyD)
- Clinical mental health specialists
Some insurers also allow psychiatric NPs or psychiatrists if the provider does not provide a medical evaluation during the visit.
Always check:
- Credentialing file
- Payer contracts
- State scope-of-practice rules
Submitting 90791 under an unapproved provider NPI almost always leads to denials.
Document the Evaluation Thoroughly
Your note must show that you performed a complete diagnostic evaluation. This is where many denials happen because clinicians under-document the session.
Include these elements clearly:
- Presenting problem: why the patient came in
- History (psych, medical, family, social, substance use)
- Mental Status Exam
- Risk assessment
- DSM-5-TR diagnostic impressions
- Functional impairments
- Treatment plan with goals
Most insurers expect 45+ minutes of clinical evaluation.
Document start and end times to avoid medical review.
Example:
“Evaluation conducted from 10:00 AM to 10:58 AM (58 minutes).”
Telehealth Requirements (Mandatory for 2025)
Add a single line for:
- Patient location
- Provider location
- Consent
- Platform used
Insurance is ruthless about missing telehealth details.
Use the Correct Place of Service (POS) Code
A wrong POS code can delay payment by weeks.
Here are the most common:
- 11: Office
- 02: Telehealth (old)
- 10: Telehealth (2025 standard — patient at home)
- 03: School
- 52: Community mental health center
For telehealth, most payers now prefer POS 10.
Link 90791 to the Appropriate ICD-10 Diagnosis
Your diagnostic impression must connect logically to the service.
Acceptable diagnoses include:
- F41.1 Generalized Anxiety Disorder
- F33.1 Major Depressive Disorder
- F43.10 PTSD
- F90.0 ADHD
- F32.A Depression, unspecified
Avoid “Z codes only” — they often get denied unless medically justified.
Check If Preauthorization Is Required
Some commercial plans require prior authorization for a diagnostic evaluation.
If needed, add the authorization number directly to the claim.
No auth = automatic denial.
Submit the Claim With All Required Elements
Your 90791 claim must include:
- CPT Code: 90791
- Provider NPI
- Tax ID
- Payer ID
- Date of service
- Place of service
- ICD-10 diagnosis
- Authorization number (if required)
- Rendering vs. billing provider (if using supervision model)
One missing field can hold up an entire claim batch.
Final Thoughts
CPT 90791 isn’t just another billing code — it’s the backbone of mental-health reimbursement.
This is the moment where you capture the full clinical story, set the direction of treatment, and establish the medical necessity that supports every future claim. When you bill it right, it pays well. When you document it correctly, it protects you from denials, audits, and uncomfortable payer questions.
But this code comes with weight.
Payers expect a proper diagnostic evaluation — not a casual conversation, not a half-filled intake, and definitely not a quick warm-up before therapy. They want a complete clinical picture: history, symptoms, risks, diagnosis, and your thought process tied together in a clear narrative.
When you master 90791 inside and out, three things happen:
- Your reimbursement becomes consistent and predictable.
- Your compliance becomes audit-proof.
- Your patients receive a clearer, stronger standard of care.
It’s the win-win every practice needs.
Struggling With CPT 90791 Denials or Documentation Issues?
ANR Medical Billing specializes in psychiatry and mental health billing services, helping providers code diagnostic evaluations correctly, avoid payer denials, and get paid faster.
We help mental-health providers:
- Code 90791 and 90792 are correct every single time
- Catch documentation gaps before claims go out
- Speed up reimbursement and reduce aging AR
- Fight denials and win back lost revenue
- Handle payer rules, provider credentialing, and compliance
- Build a cleaner, smoother intake-to-claim workflow
You focus on clinical care. We focus on getting you paid — fully, fast, and without the headaches.
