
Family psychotherapy is no longer optional in behavioral health. It is central to effective treatment. CPT code 90847 exists because mental health conditions rarely develop in isolation. Family dynamics, communication patterns, trauma exposure, and caregiver behavior often shape patient outcomes.
Still, this code creates confusion, and many providers use it casually. Payers do not see it that way. They review 90847 claims closely. Denials, downcoding, and audits are common when documentation falls short.
This guide explains CPT 90847 in a way competitors often skip. Not just what it is, but how payers interpret it, why claims fail, and how to bill it safely and profitably in today’s healthcare environment.
CPT Code 90847 Meaning and Description
CPT code 90847 describes family psychotherapy with the patient present. The emphasis is not on the family. The emphasis is on the patient’s mental health condition and how family interactions directly affect it.
The therapist actively treats the patient’s diagnosis during the session. Family members participate because their behaviors, responses, or communication patterns influence the patient’s symptoms.
This is not family counseling. It is not education. It is structured psychotherapy delivered to the patient in a family context.
The session is typically 50 minutes long, and the patient must be present for most of that time.
CPT 90847 and AMA CPT Guidelines
CPT code 90847 is defined under the Current Procedural Terminology (CPT) manual published by the American Medical Association. The code falls within the psychotherapy section and requires active treatment of the identified patient.
The key phrase in the AMA description is “with patient present.” This language is not flexible. It is a structural billing requirement.
Payers often interpret CPT guidelines conservatively, meaning documentation must clearly support:
- Active psychotherapy
- Identified patient focus
- Direct symptom treatment
Practices providing mental health billing services must ensure clinicians understand this distinction before claims submission.
Why CPT 90847 Exists in Behavioral Health Care
Behavioral health outcomes improve when families are involved appropriately. Research consistently shows better symptom control, lower relapse rates, and improved medication adherence when families support treatment.
Because of this, insurers recognize family psychotherapy as a medically necessary service when used correctly.
However, payers also know this code is abused. Many practices bill it for parent coaching, marital therapy, or family discussions that do not meet psychotherapy standards. That is why payers require strong justification.
CPT 90847 sits at the intersection of clinical care and revenue risk. Used well, it strengthens both. Used casually, it becomes a denial magnet.
CPT 90847 vs CPT 90846 – A Critical Distinction
One of the most common billing errors in behavioral health involves mixing these two codes.
- CPT 90847 applies only when the patient is present during the session.
- CPT 90846 applies only when the patient is not present.
Payers do not allow flexibility here. If the patient leaves early, joins late, or is not involved meaningfully, billing 90847 becomes risky.
A common mistake is billing 90847 for parent-only sessions with children. That is incorrect. Those sessions belong under 90846 or may not be billable at all, depending on payer rules.
Auditors often compare attendance notes with the CPT selection. Inconsistencies lead to recoupments.
Time Requirements and Session Structure
CPT 90847 is a time-based psychotherapy code. The standard expectation is around 50 minutes, with payer-accepted flexibility usually between 45 and 60 minutes.
Sessions shorter than this range raise questions. Sessions longer than this range require a clear clinical justification.
Documentation should always reflect:
- Start and stop times
- Total face-to-face psychotherapy time
- Active therapeutic work performed
Payers increasingly expect time transparency, especially for behavioral health services.
Medical Necessity of CPT 90847 Approval
Medical necessity is the deciding factor in every family therapy claim.
Payers ask one question:
How did directly involving the family help treat the patient’s condition?
Your documentation must answer that clearly.
Generic statements do not work. Saying “family support discussed” or “communication addressed” invites denial.
Instead, document how family behaviors contribute to symptoms. For example, parental reassurance reinforces anxiety, marital conflict worsens PTSD symptoms, or inconsistent discipline aggravates ADHD behaviors.
Family involvement must be essential to treatment progress, not optional.
Diagnoses Commonly Linked to CPT 90847
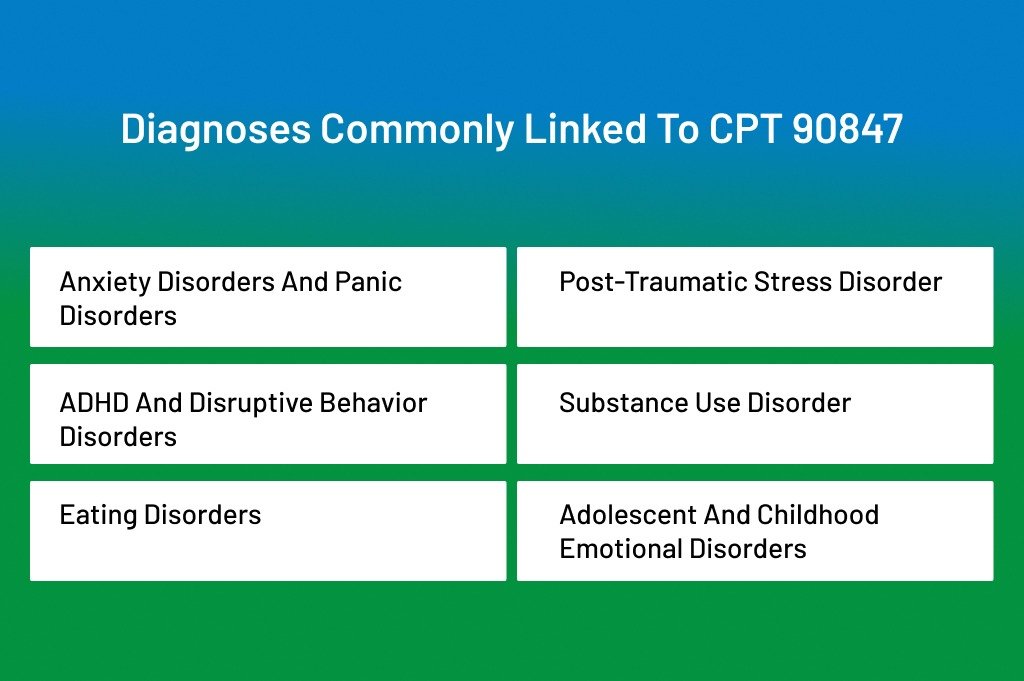
CPT 90847 is appropriate for many behavioral health diagnoses, including:
Mood disorders such as depression and bipolar disorder
- Anxiety disorders and panic disorders
- Post-traumatic stress disorder
- ADHD and disruptive behavior disorders
- Substance use disorder
- Eating disorders
- Adolescent and childhood emotional disorders
The diagnosis must belong to the identified patient. Family members’ conditions do not justify the code.
ICD-10 Diagnosis Linkage for CPT 90847
Correct ICD-10 coding strengthens medical necessity. CPT 90847 is commonly linked with:
- F33.1 – Major depressive disorder, recurrent, moderate
- F41.1 – Generalized anxiety disorder
- F43.10 – Post-traumatic stress disorder
- F90.2 – ADHD, combined type
- F31.9 – Bipolar disorder, unspecified
The diagnosis must belong to the identified patient. Z-codes for family stressors alone rarely justify reimbursement.
Accurate diagnosis-to-service linkage is a core function of high-performing behavior health billing services and reduces audit exposure.
Documentation Requirements
High-performing practices document clinical logic. Your session note should explain:
- Who attended and their relationship to the patient
- Confirmation that the patient was present
- Presenting symptoms and current stressors
- Specific family dynamics impacting symptoms
- Therapeutic techniques used
- Patient response and engagement
- Progress toward treatment goals
Notes should read like clinical narratives, not templates. Repetition across visits signals risk to payers.
Medicare Billing Rules for CPT 90847
Centers for Medicare & Medicaid Services (CMS) covers CPT 90847 when family involvement is directly related to the patient’s psychiatric treatment plan.
Medicare requires:
- Medical necessity documentation
- Patient-centered therapy
- Qualified provider credentials
- Progress tracking
Family sessions conducted solely for caregiver education are non-covered services under CMS guidelines.
Behavioral health practices that outsource to professional behavioral health billing services often see fewer Medicare denials because documentation is audited before submission.
Medicaid Coverage: State-by-State
Medicaid policies vary widely.
- Some states require prior authorization.
- Others cap annual visit limits.
- Many require detailed treatment plans and progress tracking.
Medicaid claims are often denied for missing documentation, even when services were clinically appropriate. Practices must align billing workflows with state Medicaid manuals.
Ignoring state-specific Medicaid rules is one of the fastest ways to lose revenue.
Commercial Payer Reimbursement Patterns
Commercial insurers reimburse CPT 90847 at rates comparable to individual psychotherapy codes.
Average reimbursement typically falls between $110 and $160, depending on contract terms, location, and provider credentials.
Most commercial payers require authorization for ongoing family therapy. Claims without authorization are frequently denied regardless of documentation quality.
How to Bill CPT Code 90847 – Step-by-Step Billing Workflow
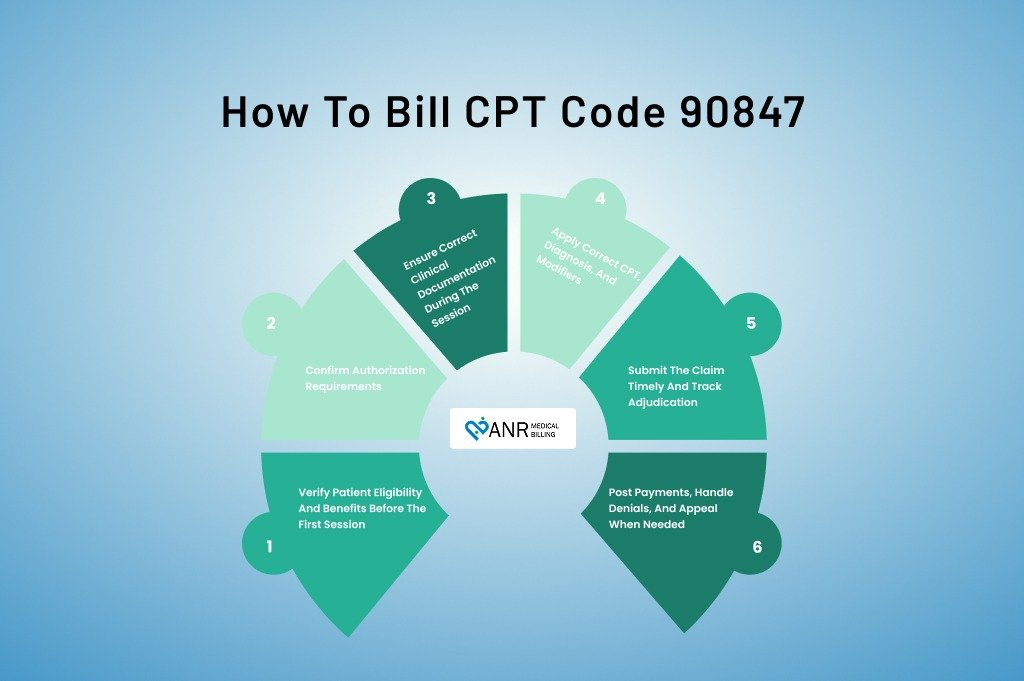
Billing CPT code 90847 is not just about selecting the correct code. It is about aligning clinical care, documentation, payer rules, and revenue cycle processes into one clean workflow. When one step breaks, the claim usually fails.
Let’s walk through the entire billing process the way successful behavioral health practices actually do.
Step 1: Verify Patient Eligibility and Benefits Before the First Session
Before family psychotherapy even begins, eligibility verification sets the tone for reimbursement.
You must confirm that the patient’s insurance plan covers family psychotherapy with the patient present. Many plans cover individual therapy but restrict family sessions. Some require prior authorization from the first visit.
At this stage, billing teams should verify:
- Behavioral health coverage details
- Family therapy benefits
- Session limits per year
- Authorization requirements
- Telehealth eligibility, if applicable
Skipping this step often results in services that go unpaid.
Step 2: Confirm Authorization Requirements
CPT 90847 frequently requires prior authorization, especially for commercial and Medicaid plans.
Authorization should match:
- The CPT code (90847 specifically)
- The diagnosis
- The provider’s credentials
- The approved number of visits
A common billing mistake is obtaining authorization for individual therapy (CPT 90834 or CPT 90837) and billing family therapy instead. Payers treat this as an invalid service, even if the treatment was clinically appropriate.
Authorization mismatches are one of the top causes of avoidable denials.
Step 3: Ensure Correct Clinical Documentation During the Session
Billing for CPT 90847 begins in the therapy room.
Clinicians must clearly document:
- The patient was present
- Who else attended the session
- The patient’s diagnosis and symptoms
- Family dynamics affecting the patient
- Therapeutic interventions used
- Patient response and progress
Documentation must show that this was psychotherapy, not education or family discussion. Patients expect to see active clinical treatment directly tied to their condition.
Generic notes are not enough. Clear clinical reasoning protects the claim.
Step 4: Apply Correct CPT, Diagnosis, and Modifiers
When submitting the claim, coding accuracy matters.
CPT code 90847 should be billed with:
- A covered behavioral health diagnosis belonging to the patient
- The rendering provider’s correct NPI
- Appropriate place of service code
- Telehealth modifiers, if applicable
If billed via telehealth, the modifier and POS rules must match the payer’s current policy. Incorrect modifiers can trigger automatic denials even when documentation is strong.
Step 5: Submit the Claim Timely and Track Adjudication
Timely filing rules still apply. Many practices lose revenue simply because family therapy claims are submitted late or not tracked at all.
After submission, monitor:
- Claim acceptance
- Payer processing time
- Payment accuracy
- Denial reasons, if any
CPT 90847 claims should never be “set and forget.” They need active follow-up.
Step 6: Post Payments, Handle Denials, and Appeal When Needed
When payment posts, confirm:
- Correct allowed amount
- Proper application of the deductible or copay
- No downcoding
If denied, appeal with:
- Session notes
- Treatment plan
- Authorization proof
- Medical necessity explanation
Well-written appeals often overturn 90847 denials when documentation supports the service.
How to Avoid CPT 90847 Billing Errors?
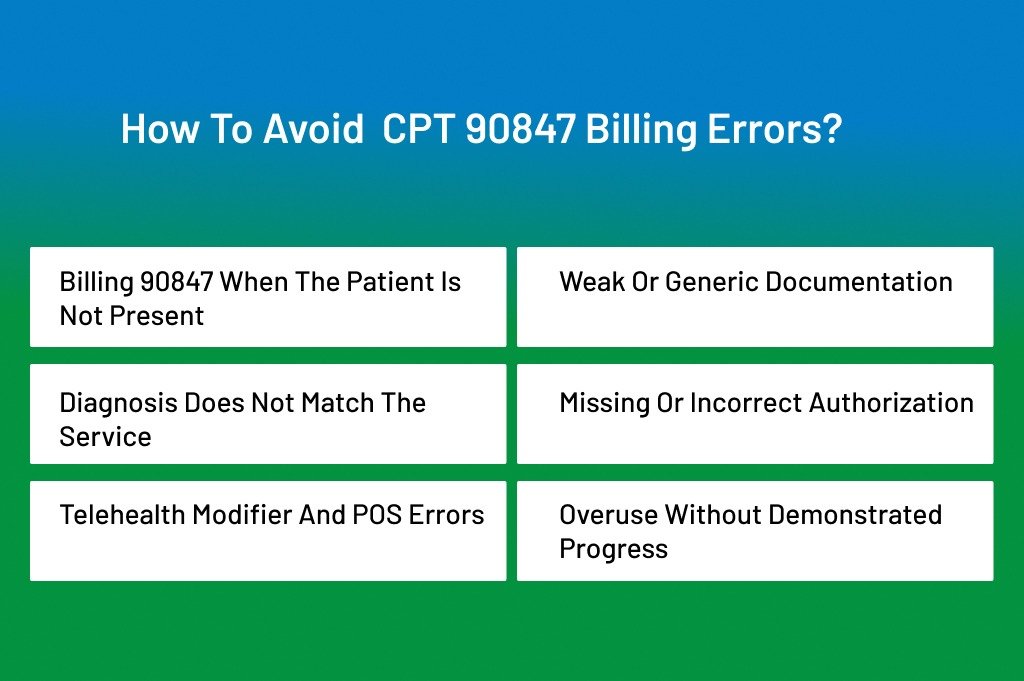
CPT 90847 errors follow predictable patterns. The same mistakes appear across practices, regardless of size. Knowing them upfront helps avoid revenue loss.
Billing 90847 When the Patient Is Not Present
This is the most frequent and costly mistake.
If the patient is not present for most of the session, 90847 is invalid. Even if parents or caregivers attend, the code requires patient participation.
How to avoid it: Train clinicians to document patient presence clearly. If the session is caregiver-only, switch to 90846 or confirm if the service is billable at all.
Weak or Generic Documentation
Payers deny many family therapy claims because notes lack depth.
Statements like “family discussed concerns” or “support provided” do not demonstrate psychotherapy.
How to avoid it: Document specific interventions, clinical reasoning, and how family dynamics affect the patient’s symptoms. Notes should read like treatment, not conversation summaries.
Diagnosis Does Not Match the Service
CPT 90847 must link to the patient’s diagnosis. Using a family member’s diagnosis or a vague Z-code often results in denial.
How to avoid it: Always bill the identified patient’s behavioral health diagnosis. Ensure diagnosis codes remain consistent with the treatment plan.
Missing or Incorrect Authorization
Many practices deliver family therapy, assuming authorization is covered under individual therapy approvals. Payers disagree.
How to avoid it: Verify that authorization explicitly includes CPT 90847. Carefully track visit counts to prevent exceeding approved limits.
Telehealth Modifier and POS Errors
Telehealth billing rules vary by payer and change frequently. Incorrect modifier use leads to fast denials.
How to avoid it: Maintain payer-specific telehealth billing guidelines. Audit telehealth claims monthly for accuracy.
Overuse Without Demonstrated Progress
Frequent use of CPT 90847 without documented improvement raises red flags.
Payers expect to see progress or an apparent clinical reason for continued family involvement.
How to avoid it: Update treatment goals regularly. Document progress, barriers, and the ongoing necessity for family therapy.
CPT 90847 and Behavioral Health Revenue Cycle Management
Family psychotherapy billing sits in a compliance-sensitive segment of behavioral health revenue cycle management.
Because 90847 requires:
- Authorization alignment
- Time validation
- Medical necessity support
- Correct modifier usage
It benefits significantly from specialized behavioral health billing services rather than general medical billing support.
Practices that integrate clinical documentation review with billing operations typically see:
- Lower denial rates
- Faster reimbursements
- Fewer audit recoupments
- Stronger payer contract performance
Frequently Asked Questions About CPT 90847
Is CPT 90847 time-based?
Yes. It typically requires 45–60 minutes of psychotherapy with the patient present.
Can 90847 be billed via telehealth?
Yes, if the payer allows telebehavioral health services and appropriate modifiers are used.
Can you bill 90847 and 90837 on the same day?
Generally no, unless distinct services are clearly documented and allowed by the payer.
Does CPT 90847 require prior authorization?
Often yes, especially with Medicaid and commercial plans.
Final Thoughts
CPT 90847 is one of the most valuable and most scrutinized psychotherapy codes. It sits in a high-risk, high-reward space.
Practices that treat it casually lose money. Practices that treat it strategically build stable revenue while staying compliant.
Strong workflows, trained clinicians, accurate coding, and proactive audits turn CPT 90847 into a reliable billing code instead of a denial headache.
When billed correctly, family psychotherapy supports better care, stronger compliance, and predictable reimbursement.
Stay Compliant. Get Paid Correctly.
CPT 90847 is high-risk and high-reward. ANR Medical Billing specializes in mental and behavioral health billing services that protect your revenue and reduce audit exposure.
Let ANR Medical Billing handle your billing while you focus on patient care.
