Medicaid billing for mental health services often feels confusing, time-consuming, and risky. One small mistake can delay payments or trigger denials. Still, Medicaid remains a major payer for behavioral health care, and many practices depend on it to stay stable.
The key is understanding how Medicaid thinks. It does not just look at codes. It seems that eligibility, medical necessity, documentation, authorization, and compliance all work together. When providers understand the entire flow, billing becomes predictable rather than stressful. This guide is built to help mental health providers see the complete picture and bill Medicaid with confidence.
How to Bill Medicaid as a Mental Health Provider
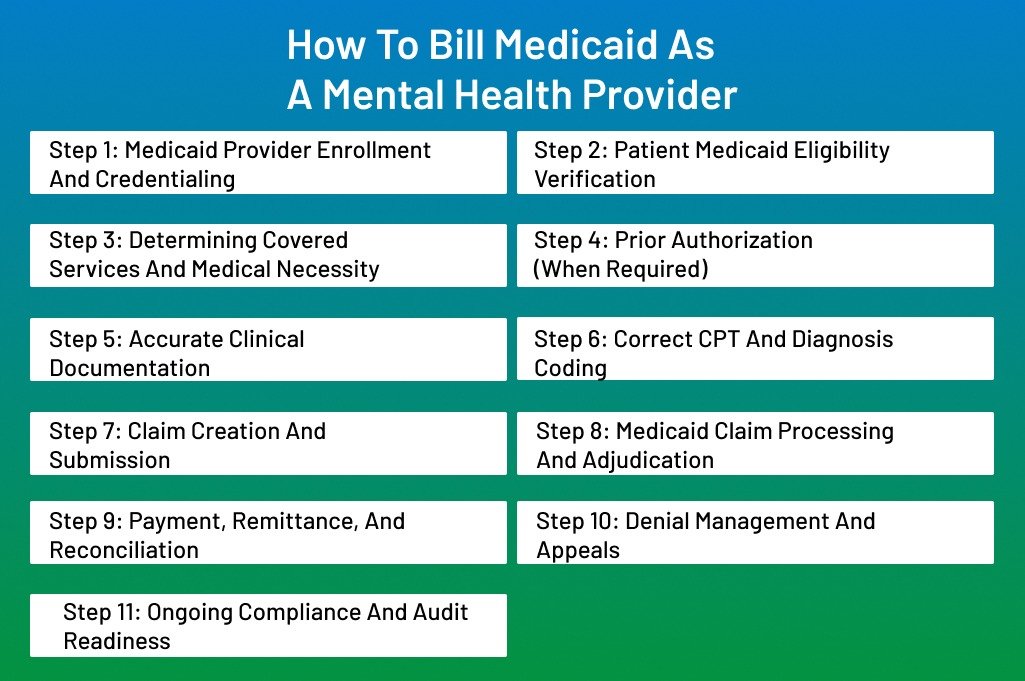
Every Medicaid claim follows a clear path. When providers understand that path before jumping into the steps, billing becomes far less stressful. Each stage builds on the one before it, from eligibility checks to final payment. Missing a single step can break the entire chain.
Let’s go into detail on how to bill Medicaid as a mental health provider.
Step 1: Medicaid Provider Enrollment and Credentialing
Everything starts with enrollment. Medicaid does not pay for services simply because they were rendered. It only pays enrolled and approved providers. This rule applies to psychiatrists, psychologists, therapists, and clinics alike.
Enrollment tells Medicaid:
- Who you are
- What license do you hold
- What services are you allowed to bill
- Whether you can bill independently or under supervision
If enrollment is incomplete or mismatched, claims are automatically denied, often without detailed explanations.
Enrollment is not just paperwork. It creates your billing identity inside the Medicaid system. Medicaid links your NPI to your license, taxonomy, supervision rules, and service scope.
For group practices, this step has two layers:
- The organization must be enrolled
- Each rendering provider must also be enrolled
One without the other results in denials.
Key enrollment elements: Medicaid checks:
- Active NPI and taxonomy
- State license status
- Provider type recognition
- Supervision requirements
- Group vs individual billing structure
Step 2: Patient Medicaid Eligibility Verification
Eligibility verification is not a one-time task. Medicaid eligibility changes often. Patients can lose coverage, switch plans, or move between fee-for-service and managed care without warning.
Medicaid pays only if the patient is eligible on the exact date of service.
Many denials happen even when services were appropriate, simply because eligibility was inactive or assigned to a different plan.
Eligibility verification also tells you:
- Which Medicaid plan covers the patient
- Whether behavioral health is carved out
- What visit limits apply
- If prior authorization is required
What should be verified before every visit:
- Active Medicaid status
- Correct Medicaid ID
- Managed care vs state Medicaid
- Behavioral health coverage details
Skipping this step leads to avoidable write-offs.
Step 3: Determining Covered Services and Medical Necessity
Medicaid does not cover services just because they are clinically helpful. It covers services that meet medical necessity criteria under state Medicaid rules.
Medical necessity connects:
- Diagnosis
- Functional impairment
- Type of service
- Frequency and duration
If these pieces do not align, claims will be denied or get recouped later.
Medicaid wants proof that:
- A diagnosable mental health condition exists
- The condition affects daily functioning
- The service directly addresses that condition
- Ongoing treatment is justified
This logic must be visible in the chart, not assumed.
Common medical necessity pitfalls include:
- Vague diagnoses
- High-frequency therapy without progress
- Notes focused only on emotions
- No updated treatment plan
Step 4: Prior Authorization (When Required)
Prior authorization is Medicaid’s way of controlling utilization. Not every service requires it, but when it does, skipping authorization almost always results in non-payment.
Authorization rules vary by:
- State Medicaid program
- Managed care plan
- Service type
- Visit frequency
Although rules differ, authorization is often required for:
- Psychological and neuropsychological testing
- Extended or high-frequency therapy
- Intensive outpatient services
- Crisis stabilization programs
Authorization approval must be obtained before services are rendered, not after.
Authorization details Medicaid checks:
- Valid authorization number
- Approved service type
- Allowed visit count
- Authorization date range
Providing services outside approved limits leads to denials.
Step 5: Accurate Clinical Documentation
Documentation is the backbone of Medicaid billing. Coding gets the claim through the door. Documentation decides whether it stays paid.
Medicaid documentation must show why the service was needed, what was done, and how it helped.
Each encounter note should clearly include:
- Date and duration of service
- Service type and location
- Presenting problem
- Interventions used
- Patient response
- Progress toward treatment goals
- Provider signature and credentials
Treatment plans must support the frequency and type of care. Outdated or missing plans are one of the top audit findings.
Step 6: Correct CPT and Diagnosis Coding
Coding translates clinical care into billable data. Medicaid expects codes to match documentation exactly.
Mental health CPT codes are often time-based. Medicaid checks whether:
- Documented time supports the code
- Services billed match provider scope
- Therapy and evaluation codes are not misused
Overcoding or undercoding both create problems.
Diagnosis codes must:
- Support medical necessity
- Align with the treatment plan
- Stay consistent across visits
Frequent changes in diagnosis without explanation raise red flags.
Step 7: Claim Creation and Submission
Once documentation and coding align, the claim can be created. Medicaid claims are unforgiving. Small errors lead to rejections.
A clean claim includes:
- Patient Medicaid ID
- Correct billing provider NPI
- Correct rendering provider NPI
- CPT and ICD-10 codes
- Place of service
- Date of service
Claims are typically submitted electronically through clearinghouses or state portals.
Step 8: Medicaid Claim Processing and Adjudication
After submission, Medicaid reviews the claim against:
- Eligibility records
- Enrollment files
- Authorization systems
- Coding edits
- Policy rules
Claims may be:
- Paid
- Denied
- Rejected (never entered processing)
Understanding denial codes is key to fixing issues quickly.
Step 9: Payment, Remittance, and Reconciliation
When Medicaid pays, it issues a remittance advice explaining:
- Allowed amount
- Paid amount
- Adjustments or denials
Medicaid payment is the final payment. Balance billing patients is not allowed.
Practices must match payments to claims. Unreconciled payments hide underpayments and denials.
Reconciliation helps identify:
- Missing payments
- Incorrect reimbursements
- Systemic billing errors
Step 10: Denial Management and Appeals
Denials are part of Medicaid billing. Ignoring them leads to revenue loss.
Common Medicaid Denial Causes
Most denials stem from:
- Eligibility issues
- Missing authorization
- Provider enrollment mismatches
- Documentation gaps
- Supervision errors
Appeals must be filed within strict deadlines. Successful appeals rely on:
- Corrected claims
- Supporting documentation
- Clear explanations
Tracking denial trends prevents repeat problems.
Step 11: Ongoing Compliance and Audit Readiness
Medicaid audits do not only target unpaid claims. Paid claims are reviewed months or years later.
Auditors review:
- Documentation quality
- Treatment plan consistency
- Authorization compliance
- Provider scope adherence
- Supervision proof
Strong internal processes protect against recoupments.
Final Thoughts
Medicaid billing works best when it is treated as a connected system rather than a set of isolated tasks. Eligibility checks protect services before they start. Clear documentation supports medical necessity. Correct coding aligns with the provider scope. Authorization keeps claims payable. Follow-up and compliance protect revenue long after payment is posted.
When these pieces stay aligned, denials drop, and cash flow improves. More importantly, providers gain time and peace of mind. Instead of chasing claims, they can focus on patient care, knowing their billing stands on solid ground.
Simplify Medicaid Billing With ANR Billing
Medicaid billing does not have to drain your time or energy. At ANR Billing, we handle the entire Medicaid mental health billing lifecycle with precision and care. Our team understands provider-specific rules, state Medicaid policies, and payer behavior that causes denials.
We work behind the scenes to keep your claims clean, compliant, and paid—so you can focus on what matters most.
What ANR Medical Billing Supports
- Medicaid enrollment and revalidation
- Eligibility and authorization management
- Accurate mental health coding
- Documentation and compliance review
- Denial resolution and appeals
- Ongoing audit readiness
If Medicaid billing feels overwhelming, it is time to bring in experts who live and breathe it every day.
Frequently Asked Questions (FAQs)
How long does Medicaid take to pay mental health claims?
Payment timelines vary by state and by plan type. In most cases, clean Medicaid mental health claims are processed within two to four weeks. Managed Medicaid plans may take slightly longer. Delays usually happen when eligibility, authorization, or documentation details are missing or unclear.
Do mental health providers need to verify Medicaid eligibility for every visit?
Medicaid eligibility can change monthly or even mid-month. Verifying eligibility before each visit helps prevent denials caused by inactive coverage or plan changes. This step also confirms whether the patient is in a managed care plan and if authorization rules apply.
Does Medicaid require prior authorization for all mental health services?
Not for every service. Routine therapy sessions may not need authorization, but services like psychological testing, high-frequency visits, or intensive programs often do. Authorization rules depend on the state Medicaid program and the patient’s managed care plan.
What documentation does Medicaid expect for mental health billing?
Medicaid expects detailed session notes that explain medical necessity. Notes should include the service date, time spent, interventions used, patient response, and progress toward treatment goals. An active treatment plan that supports the frequency of care is also required.
Can Medicaid take back payments after claims are paid?
Medicaid conducts post-payment audits regularly. If documentation, authorization, or supervision requirements are not met, Medicaid may request refunds. Strong documentation and consistent compliance help reduce this risk.
